Do you have sleep apnea?
“OSA [Obstructive Sleep Apnea] affects nearly 30 million Americans, and 80% of cases are undiagnosed.”
— The Obstructive Sleep Apnea (OSA) National Indicator Report
According to this report, sponsored by a grant from the CDC, a general lack of awareness is the primary driver behind the 23.5 million untreated cases of obstructive sleep apnea (OSA) and $149.6 billion annual cost due to increased health care utilization, motor vehicle and workplace accidents, and reduced productivity in the United States alone. In other words, we as Americans aren’t talking about it. So, in the spirit of educating others via this Substack, I wanted to talk about my experiences with my obstructive sleep apnea diagnoses, treatment, and struggles (!!) from a personal perspective.
Like all the Wednesday “B-sides” posts, this topic was inspired by a friend. It was a short chat over Facebook Messenger a couple months ago:
Before you leave this post, remember that OSA is not just limited to those who are overweight or obese. And, it turns out the risks of OSA in non-obese patients are significant when compared to simply being obese without OSA.
Approximately 20% of adults with OSA are non-obese. OSA in non-obese patients is usually less severe and less frequent. However, it is essential to identify these patients because they are four times more likely to develop hypertension than obese without OSA. Non-obese patients are at risk for early atherosclerosis approximately 2.7 times more than obese patients without OSA, and this risk increases as the severity of the syndrome increases.
— Antonaglia & Passuti (2021) “Obstructive sleep apnea syndrome in non-obese patients”
So, I’ll use this space to share my own story, and I’d appreciate hearing yours, too.
UPDATE: Paywall removed for Christmas 2024!
The rest of this post is behind a “paywall”. (“Paywall” is in quotation marks because I value engagement more than the subscription fees!) I will “comp” you one month of “paid” subscription if you leave a chat using the link above, if you message me or refer friends to subscribe to this Substack using the links below.
Or, if you don’t want to bother, feel free to try a paid subscription free for 30 days. If you go on to pay, you’ll be treating me to beer or coffee!
I first referred to my sleep apnea in my post Feelings that Persist. In that post, I reflected about how our marital conflict over my snoring wasn’t really about snoring. In this post, I want to talk about snoring!
Sleep apnea can creep up
Even though I did snore heavily most of my adult life, my original diagnosis was my oxygen level stayed above 95% and that insurance wouldn’t cover any treatment.
About half the people who snore do not have sleep apnea.
“What we call primary snoring is snoring without sleep apnea, so the tissues vibrate, and they make the noise, but the person is still getting sufficient air and it’s not disrupting the person’s sleep. Snoring can disrupt a bed partner or other people in the house, but primary snoring would not affect the person who’s doing the snoring.”
— Virginia Skiba, neurologist and sleep medicine physician, Henry Ford Medical Center
So, I thought I was good, right? No!
As time progressed, my results changed. In fact, sleep apnea is more common in middle-aged and older adults. As people age, fatty tissue can build up in the neck and the tongue and raise the risk of sleep apnea.
In my case, my Type 2 diabetes and insulin resistance could have played a role, too. High levels of the insulin hormone can affect the size and shape of the face, tongue, and airway.
For me, the trigger came during a normal visit to UCSF in 2023 as part of an observational study as a “cognitively normal” control for dementia. I recalled to the neurologist there about how I sometimes have lapses in memory, and he recommended I take another sleep study. The results now showed that my oxygen level had gotten as low as 71%! (It should remain above 90%.)
So, the snoring was constant, but the sleep apnea just crept up on me as I aged! There is a wide body of literature that shows how sleep apnea can impact memory and cognitive decline. This was an area to be taken seriously given the low oxygen levels.
AHI
One term the doctors use to describe the severity of sleep apnea is AHI or Apnea-Hypopnea Index. The full explanations are available online. Basically, it’s a measurement of how many times a person's breathing stops or slows during sleep.
In my case, my AHI was 13.4.
The basic “guide” here to AHI is as follows:
Normal sleep: An AHI of fewer than five events, on average, per hour
Mild sleep apnea: An AHI of five to 14 events per hour
Moderate sleep apnea: An AHI of 15 to 29 events per hour
Severe sleep apnea: An AHI of 30 or more events per hour
Still, even though my sleep apnea when considering AHI was “mild,” it was really my lowest saturation at 71% that was considered severe and that needed medical attention.
Insurance pays for this
With this sleep study result, my insurance plan covered my treatment. Here was the process I went through:
My primary care physician (PCP) referred me to OHSU Sleep Medicine.
After reviewing my sleep study, my sleep medicine doctor prescribed a CPAP. Because of the severity of my oxygen deprivation, I was steered away from a dental appliance as an option.
I was contacted by Norco, a medical equipment supplier to arrange for CPAP delivery.
Once the CPAP arrived, I had to use it for at least 4 hours per night on 70% of nights for the next 30 days (i.e., 21 nights). The CPAP machine itself communicates over the cellular network, so my doctor at OHSU could also see the results.
I had to schedule an appointment with my sleep doctor at OHSU after the 31st day to both validate usage, as well as to verify that the treatment was working. My AHI was measured at 1.18, which is in the “normal” range. To validate my blood oxygen levels, a Virtuox overnight oximetry testing kit was sent to me at home. (The $50 for this test was NOT covered by insurance, as the supplier was “out of network.”)
My nocturnal oximetry results showed that my blood oxygen was staying above 90%, so the treatment was deemed to be working.
Once everything got validated, my insurance started paying the medical equipment supplier $47.27 per month on CPT code E0601RR. (The actual billed fee was $122.25 per month, with a provider discount of $74.98! All of this stuff is heavily marked up above what insurance really pays.)
In addition, the medical equipment supplier sends me an ongoing subscription of supplies, all covered by insurance. Now, every 3 months, I get a new tube (A4604NU, $47.47), a new face mask (A7304NU, $64.60), and a 3 month supply of filters (A7038NU, $15.46) and nasal pillows (A7033NU, $109.51) . After 6 months, I also received a new headgear (A7035NU, $21.67) and a humidifier water tub (A7046NU, $15.68). I’m only 9 months in, so I don’t know what other stuff I will be getting in the mail in future installments!
Gamification
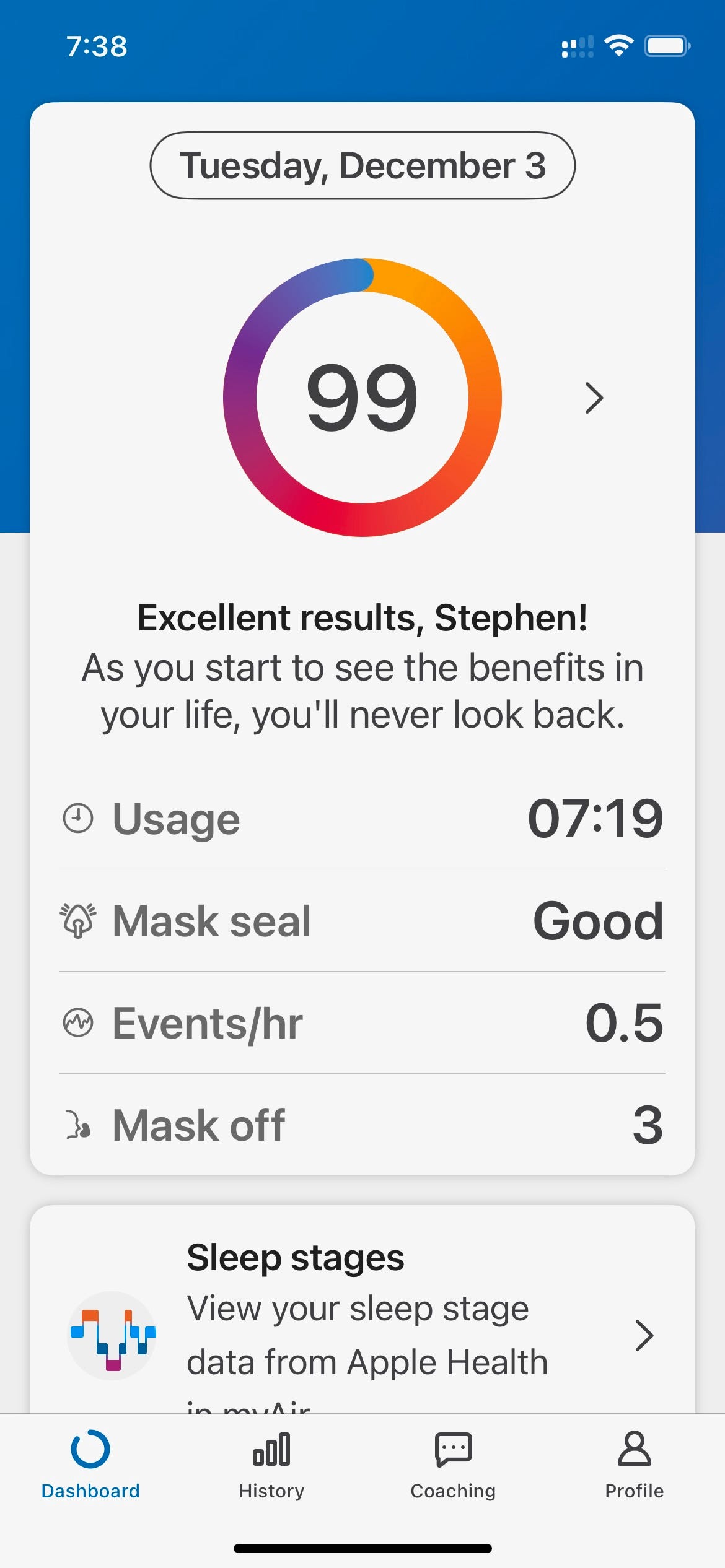
While the pulse oximetry was a one-time test, there is ongoing gamification that the CPAP provides. The accompanying myAir app monitors usage, the mask seal, the “events / hr” (similar to AHI), and the number of times the mask was off. (Unfortunately, I usually have to pee at night because of my Jardiance prescription, so I will almost always have “mask off” events). This was a screen shot I took this morning!
So, overall, this has been shown to medically work, and the gamification works well for me.
Mask type
The choice people have to make is the mask type: nasal pillows, nasal mask, or full-face mask.
Image source: sleepdr.com
I am using nasal pillows. Nasal pillows are made out of a soft silicone and sit slightly inside the nostril. The difference between my configuration and those pictured is that the air flows through air channels in the face mask itself and then through a tube on the top of the head gear.
The challenge with the alternative of not having the tube on the top of the head but instead in front similar to an “elephant trunk” is that the tubing can get in the way. My friend who uses this “elephant trunk” configuration installed a hanger over his bed to keep the tubing out of the way.
The face mask with the tube on top of the head does not require a hanger like this. I took this selfie this morning, too.
Overcoming Struggles
Still, I am 9 months into the CPAP therapy, and I still must admit that I’m still not 100% used to it. Here are some struggles that I have had with it and how I have managed through them so far.
Settings. The default settings of the machine needed tweaking. I have a ResMed Airsense 11 AutoSet. It doesn’t apply “continuous” pressure but actually adjusts the air pressure automatically on a breath-by-breath basis. The default starting setting of 5.0 was too low, and I didn’t feel I was getting enough air when first going to sleep, so my sleep doctor adjusted the starting setting to 6.2 to relieve some anxiety.
I was also finding that the maximum pressure seemed too high which would wake me up, so we tamped down the maximum setting from 15 to 10.
I’m still not sure I am 100% happy with this, but the technology is probably doing what it should be doing.
Stuffed nose. I have had allergies since I was a kid, and my nose is often too stuffed to use the nasal pillows effectively. I also know that there are full facial masks to allow for mouth breathing, but I’ve decided to hang with the nasal pillow technology for now to avoid claustrophobia. One suggestion here is to use a nasal spray, which I procured. Oxymetazoline HCL is effective, but shouldn’t be used for multiple days in a row.
Anxiety. Sometimes, I just fear not being able to get enough air when going to bed or fear getting woken up when the pressure gets too great. It makes me not want to go to sleep. I’ve found that Marsha snuggling up to me when going to bed or taking Baldrirapan (Valerian Root) can help to relieve this anxiety.
Travel. The CPAP machine is sort of big. I have started using a larger duffle that fits my CPAP machine, along with my laptop, headphones, chargers, and other accessories instead of carrying a laptop bag while traveling. I also know there are smaller travel CPAP machines which insurance does not cover. The recommended one for me was the ResMed AirMini given that I already have a ResMed AirSense 11. I think if I had to travel for business, I would likely buy one. As a retired guy, I just carry the big CPAP machine with me in the larger duffle.
Summary
For me, this journey of managing my sleep apnea started with the snoring but became a medical necessity once I started complaining of memory lapses with a neurologist. This is very serious stuff.
I was just one of many people for whom normal snoring ultimately turned into sleep apnea. I would recommend for anyone who has been checked in the past but is still wondering about sleep apnea to check again. Insurance does cover the diagnosis and this treatment.
Remember, it is estimated that 80% of cases of sleep apnea remain undiagnosed, and it is costing us greatly.
Admittedly, the solutions aren’t great. I have adjusted (somewhat) to CPAP therapy, and I wish there were a better option for someone in my situation. Still, as time has gone on, it does seem to work. I have also found some solace in being able to share the experiences with friends who have dealt with sleep apnea as well. I hope my sharing this helps you, too!